Multidisciplinary team meetings: what does the future hold
for the flies raised in Wittgenstein’s bottle?
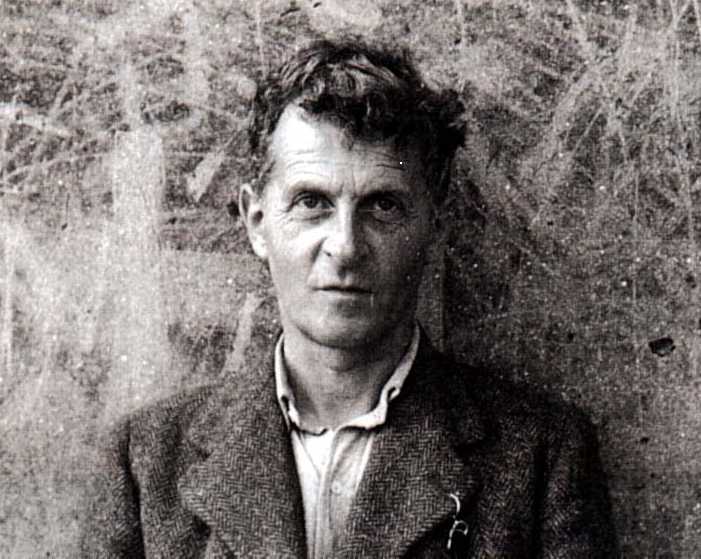
Ludwig Wittgenstein , filosofo : Vienna 1889-Cambrige 1951
fonte Lancet Oncology vol 10, febbraio 2009 pp 98-99
Do multidisciplinary cancer team meetings compromise
patients’ autonomy and the training of junior doctors?
Multidisciplinary team (MDT) meetings bring together
health-care professionals with specialist knowledge
of diagnosis and treatment. In oncology, this should
include surgeons, diagnostic and therapeutic radio-
logists, histopathologists, medical and clinical onco-
logists, nurse specialists, dietitians, psychologists, and
palliative-care physicians. At least 80% of all cancer
cases in England are thought to be discussed at MDT
meetings.
1
It has also been argued that every specialist
attending an MDT meeting is legally responsible for
their area of expertise, because it pertains to the group
decision that is reached, even if the specialist does not
speak during the meeting.
2
There can be no doubt that the establishment of MDTs
has improved coordination and communication between
departments within hospitals and between hospitals
involved in joint meetings. The purpose of this article is
to discuss two “off -target” eff ects of the homogenous
adoption of MDTs as the routine standard of care in the
UK and to make a personal plea for two action points.
First, rather than discuss treatment options with an
individual patient in the clinic, it is not uncommon
for current oncology and surgical trainees to defer to
a higher body that is scheduled to meet at a later date.
Furthermore, trainees who have no active role in the
MDT are unlikely to develop independence of thought,
critical appraisal of treatment options available to
them, and the individuality of mind that comes with
making one’s own clinical decisions, observing the
results of one’s own clinical mistakes, and learning
from them. Publication of The Tractatus3
was an
important event in philosophy. In it, Wittgenstein
describes the principles of symbolism and the relations
between words and things that are necessary in
any language. Of note, Wittgenstein states “What
fi nds its refl ection in language, language cannot
represent”.
3
The deliberations of the MDT do not have
the same meaning for an individual who experiences
decision making with patients as compared with an
individual who does not. It should be remembered
that teaching involves conveying information whereas
learning requires engagement from the student
receiving the information. There is no substitute for
the active learning achieved when a trainee must
analyse the evidence base relevant to a patient and
speak confi dently and clearly with the patient and
with members of the MDT. Indeed, MDTs off er rich
opportunities for the education of trainees and medical
students, a feature that is currently forgotten in these
frenetic business meetings that often run beyond their
allocated timeslots.
The second issue we wish to address is the key
ethical principle of respect for patient autonomy.
It has been argued that, where all else is equal (eg, a
case where there is no robust evidence base from
clinical-trial data), autonomy should take precedence
over other ethical principles.
4
As autonomy has taken
centre stage, the structure and goals of the medical
consultation have come under scrutiny. An ideal
developed in general practice, but widely applied and
taught in hospital medicine, describes the consultation
as a “meeting of equals”, between the patient, as an
expert in their own experiences and goals, and the
Democratic Forum model
Patient told diagnosis and
stage of illness. Treatment
options will be discussed at
next clinic appointment.
Patient told diagnosis and
stage of illness. Treatment
options discussed and patient’s
views of various treatment
options documented.
MDT advocates single best
treatment option based on
majority view.
MDT presentation with
clear expression of patient’s
views about treatment options.
Range of possible options
discussed with MDT, with
documentation of provisos
regarding potential detriment
of certain options and named
specialists’ formal dissension.
If declined, patient’s case
might require discussion at
MDT meeting again.
Patient can accept or decline
offer of single best treatment
option. If accepted, treatment
is implemented.
MDT opinions presented to
patient. Decision making
done in clinic with patient.
This model presumes that decision making is con cen-
trated in the consultation.
Multidisciplinary teams have set local clinical stand-
ards, and we believe that important aspects of decision
making have ceded from the doctor–patient consultation
to the MDT meeting. In many cases, the consultation
with the patient might be used only to discuss the
outcome of deliberations by a specialist professional
and to gain the patient’s consent to proceed with the
best treatment option determined by committee. In
extreme cases, the doctor’s role is to present the MDT’s
majority decision rather than the consultant’s personal
opinion of various treatment options based on their own
knowledge and experience. Does this alter the patient’s
view of the professional in front of them?
We suggest the following actions to protect patient
autonomy and to educate trainee doctors. Recognising
that attendence of all patients at MDT meetings is
not a practical solution, individual teams should take
steps to include the patient’s perspective in the initial
presentation of the clinical case and in the decisions
that are reached. In a small number of MDTs in the UK,
such an approach is already considered best practice.
Teams can encourage the presence of individuals,
such as specialist nurses or a informed doctor, who have
consulted the patient explicitly, to act as their advocates
in the MDT meeting. The chairperson of the meeting,
who might be a specialist nurse or another individual
who is not biased towards a particular treatment,
should ensure that the loudest voice in the room does
not prevail in every case. Indeed, rather than a single
treatment recommendation based on the majority
view (fi gure), the team should be willing to advocate
a range of options that could be tailored to a patient’s
preferences in the subsequent consultation, albeit with
discussion of the potential detriment of not consenting
to the “gold standard” defi ned by the MDT. Moreover,
the doctor’s perspective might have to change. The
doctor with legal responsibility for the patient’s
treatment might consider the MDT as an interactive,
individualised source of approval. The MDT’s input
could be critically applied to each situation after the
consultation with the patient in which various options
are discussed and before the consultation in which
decision making takes place.
Most importantly for trainees, there should be time
allocated at the end of the MDT meeting for debriefi ng,
discussion of educational points, and for the opinions of
medical students and trainees to be heard. Trainees and
students should be set tasks to complete before the next
MDT meeting, that involve analysis of the evidence,
communication with the patient, and presentation
of fi ndings. Team working could be encouraged by
allocating tasks to small groups. Health professionals’
time is limited and costly, so the educational sessions
could be undertaken by a designated individual after the
other MDT professionals have left the meeting. This goal
can only be achieved if resources are allocated to protect
the time of the individuals involved.
Individuality of mind requires performance of the
deed and the ability for lateral thinking. Wittgenstein
described a fl y in a bottle, which buzzes against the glass
and cannot escape. Yet there is no stopper in the bottle;
the fl y needs to add a new direction to its fl ight. Perhaps
now is the time for us to add an educational dimension
to MDTs and let our fl ies fi nd their own way out of the
bottle.
Ricky A Sharma*, Ketan Shah, Eli Glatstein
Gray Institute for Radiation Oncology and Biology, University of
Oxford, Oxford, UK (RAS); Oncology Department, Churchill
Hospital, Oxford Radcliff e Hospitals NHS Trust, Oxford, UK
(RAS, KS); Department of Radiation Oncology, University of
Pennsylvania, Philadelphia, PA, USA (EG)
ricky.sharma@rob.ox.ac.uk
Bibiography.
1 Fleissig A, Jenkins V, Catt S, Fallowfi eld L. Multidisciplinary teams in cancer
care: are they eff ective in the UK? Lancet Oncol 2006; 7: 935–43.
2 Sidhom MA, Poulsen MG. Multidisciplinary care in oncology: medicolegal
implications of group decisions. Lancet Oncol 2006; 7: 951–54.
3 Pears DF, McGuinness BF. Tractatus logico-philosophicus (translation).
London: Routledge and Kegan Paul, 1961.
4 Gillon R. Four scenarios. J Med Ethics 2003; 29: 267–68.
5 Tuckett D, Boulton M, Olson C, Williams A. Meetings between experts:
an approach to sharing ideas in medical consultations. London: Tavistock
Publications, 1985.
6 Blazeby JM, Wilson L, Metcalfe C, Nicklin J, English R, Donovan JL. Analysis
of clinical decision-making in multi-disciplinary cancer teams Ann Onc 2006, 17: 457-60
:::::: Creato il : 03/10/2009 da Magarotto Roberto :::::: modificato il : 03/10/2009 da Magarotto Roberto ::::::